[Interview] Advancing Off-the-shelf Cellular Medicines to Fight COVID-19
Mesoblast Limited (Nasdaq:MESO; ASX:MSB), a world leader in developing allogeneic (off-the-shelf) cellular medicines, just announced that the first COVID-19 infected patients have been dosed with remestemcel-L, the company’s proprietary allogeneic cellular medicine. This study is conducted within the framework of the 300-patient randomized placebo-controlled Phase 3 trial underway in North America which focuses on patients with moderate to severe acute respiratory distress syndrome (ARDS) on ventilator support.
 We talked to Dr. Fred Grossman, Chief Medical Officer with Mesoblast, to learn more about the mechanism of action for the company’s proprietary cells, and new developments to test the cells in patients with COVID-19.
We talked to Dr. Fred Grossman, Chief Medical Officer with Mesoblast, to learn more about the mechanism of action for the company’s proprietary cells, and new developments to test the cells in patients with COVID-19.
Andrii: Can you introduce yourself, and briefly outline your journey with Mesoblast?
Fred: Before joining Mesoblast about nine months ago, I held senior leadership positions in the pharmaceutical industry for close to 25 years at large (Lilly, J&J, BMS) and smaller (Sunovion, Glenmark) pharmaceutical companies developing and launching numerous drugs in areas of unmet medical need. I wanted to be part of an innovative cutting-edge, scientifically-based company poised to advance treatment for the most severe inflammatory diseases.
It has been a privilege to be part of Mesoblast’s transformation and rapid growth. We are preparing for our first cell therapy product launch - RYONCIL™ (remestemcel-L) for steroid refractory acute graft versus host disease (SR aGVHD) in children - which is currently under priority review by the US FDA. SR aGVHD is associated with a high mortality rate and occurs in more than 50% of blood cancer patients following an allogeneic bone marrow transplant. This disease is a result of severe inflammation that produces a “cytokine storm”, primarily in the skin, gut and liver. The cytokine storm in acute GVHD is similar to the mechanism responsible for COVID-19 ARDS which attacks the lungs.
Based on this and additional proof of concept, including data from a randomized controlled trial in chronic obstructive pulmonary disease (COPD) that will be presented at the upcoming 2020 annual meeting of the International Society for Cell & Gene Therapy (ISCT), we rapidly pivoted towards expanding our pipeline to include moderate to severe COVID-19 ARDS.
This is biopharma at its best--using state of the art science and nimble decision-making to create an extensive and definitive clinical development program that can possibly lead to approvals in various COVID-19 indications.
Our existing programs in adult SR aGVHD, chronic GVHD, biologic-refractory Crohn’s disease, rare diseases such as hypoxic ischemic encephalopathy, coupled with our planned Phase 3 data read-outs for our advanced heart failure and chronic low back pain programs this year creates an exciting journey as we address some of the most severe human disorders that remain resistant to conventional standard of care.
Andrii: Mesoblast is known as a leader in developing “off-the-shelf” cellular medicines. Can you name some key drivers that helped you get there? What’s the core innovation, or strategic advantage, that secures the company’s position in the industry?
Fred: Over the years, Mesoblast has created scalable allogeneic “off the shelf” mesenchymal lineage cell product candidates that meet the most stringent quality assurance requirements to produce potent, consistent and reproducible cell lines sufficient to meet near-term commercial needs. The patent estate is robust, covering composition of matter, manufacturing, and therapeutic applications, allowing strong global protection and freedom to operate. We believe the Company’s advanced manufacturing capabilities, intellectual property strength, and the potential launch of RYONCIL later this year, position Mesoblast well ahead of any competitors.
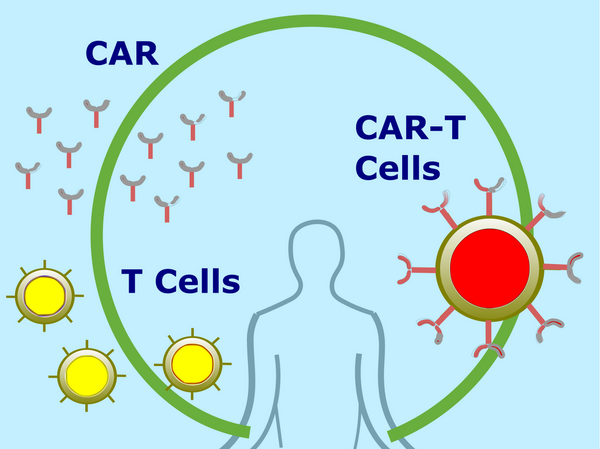
The key driver to our success is the potency of the cells, which counteract the inflammatory processes implicated in these diseases by down-regulating the production of pro-inflammatory cytokines, increasing production of anti-inflammatory cytokines, and enabling recruitment of naturally occurring anti-inflammatory cells to involved tissues in various organs. These rare cells then act on multiple arms of the immune system, including macrophages, inflammatory T-cells, and B-cells to orchestrate an anti-inflammatory response. Essentially, the cells respond to the inflammatory environment, in contrast to existing treatments which either affect one arm of the immune system or completely cut off immune function, which can lead to severe side effects. These mesenchymal lineage cells also have reparative factors.
Taken together, the proprietary manufacturing process, patent estate, potent mechanism or action, and our advanced pipeline positions us to lead the industry.
Andrii: What is the research rationale behind the use of allogeneic cellular medicines in COVID-19 ARDS patients?
Fred: Covid-19 ARDS occurs following a viral infection in the lungs which triggers alveolar inflammatory macrophages resulting in a cytokine storm caused by an influx of inflammatory cells. This damages the alveolar lung tissue. The resulting severe inflammation and fluid build-up impairs oxygen exchange, leading to hypoxemia or difficulty in breathing. Many of these patients end up on mechanical ventilation, which has a very high mortality rate. There is preclinical and clinical evidence for mesenchymal stem cells treating viral induced inflammatory lung disease, including COVID-19 ARDS, by taming the cytokine storm occurring in the lungs.
In fact, Mesoblast provided cells to The Mount Sinai Hospital in New York City to treat patients with moderate to severe COVID-19 ARDS who were on ventilators under FDA-sanctioned emergency compassionate use. Twelve patients received two intravenous infusions of remestemcel-L within the first week and nine of 12, or 75%, were removed from the ventilator over a median of 10 days and have been discharged from hospital. These promising results contrast with only 9% of ventilator-dependent COVID-19 patients being able to come off ventilators with standard of care treatment and only 12% survival in ventilator-dependent COVID-19 patients at two major referral hospital networks in New York during the same time period. The compassionate use treatment experience informed the design of the clinical protocol for the current Phase 3 randomized, placebo-controlled trial.
Andrii: Following Mesoblast’s recent announcement of dosing the first COVID patients with remestemcel-L, can you comment on your expectations at this point, and outline some plans for the nearest future developments?
Fred: We are very pleased there was an efficacy signal consistent with the expected mechanism of action in the patients treated with remestemcel-L under emergency compassionate use at Mt Sinai. However, a definitive determination of the effectiveness of this treatment can only be accomplished with a randomized placebo-controlled clinical trial (RCT). A Phase 3 multi-center RCT is well underway, with patients already randomized across leading medical centers in the US. This study is expected to enroll 300 patients across around 30 medical centers in the US and Canada comparing remestemcel-L plus maximum standard of care to placebo plus maximum standard of care. The primary efficacy outcome is mortality during the first 30 days with additional efficacy and safety measures collected.
Andrii: If the trial is successful, how long will it take until it is available for the end-users (medical facilities, patients)? Which markets you are targeting with this development?
Fred: The COVID-19 ARDS trial is expected to complete enrollment within the next four months. The trial allows for interim analyses by an independent board to determine if the trial should be stopped early for substantial efficacy or futility. The design of the trial was based on discussions with the FDA, which advised on specific design and statistical characteristics. If the trial is successful and stops early for efficacy or at completion, we would hope to have an opportunity to discuss with the FDA potential approval in moderate to severe COVID-19 ARDS in the US. We would also plan for approvals in other geographical jurisdictions.
If you liked this post -- share it with your network to help us spread the word!
Subscribe to our monthly updates to stay tuned for new companies, innovations, market reports, news, and trends in the life sciences.
Topics: Novel Therapeutics