Current Trends in Nanomedicine: Notable FDA Approvals and Clinical Trials to Follow
Nanomedicines, as it goes from the name, are nanotechnology-based drugs, used for the treatment, diagnosis or prevention of various diseases. But is “nano” defined just by the size? According to FDA, nanomedicines are the products in the nanoscale range (meaning at least one size dimension being around 1-100 nm) that can exhibit chemical or physical properties, or biological effects which differ compared to larger-scale counterparts. At the same time FDA adds that products outside the mentioned nanoscale range also can be called nanomedicines if they can exhibit similar properties or phenomena attributable to a 1-100 nm scale dimension.
Usually, nanomedicines consist of a carrier and a drug, where the last is also called an active pharmaceutical ingredient (API). However, sometimes the API can be transformed into a nanomedicine itself via manufacturing it in nanoscale size range ( stabilized nanoscale crystals). Notably, the last FDA approval of such nanocrystal drug was in 2015, which is the drug for a rare progressive lung disease. In this article we will focus on some nanomedicines approved by the FDA in the last 5 years, as well as discuss promising ongoing clinical trials.
image credit: Love Employee iStock
What are nanomedicines and what makes them nano?
Nanomedicines, as it goes from the name, are nanotechnology-based drugs, used for the treatment, diagnosis or prevention of various diseases. But is “nano” defined just by the size? According to FDA, nanomedicines are the products in the nanoscale range (meaning at least one size dimension being around 1-100 nm) that can exhibit chemical or physical properties, or biological effects which differ compared to larger-scale counterparts. At the same time FDA adds that products outside the mentioned nanoscale range also can be called nanomedicines if they can exhibit similar properties or phenomena attributable to a 1-100 nm scale dimension.
Usually, nanomedicines consist of a carrier and a drug, where the last is also called an active pharmaceutical ingredient (API). However, sometimes the API can be transformed into a nanomedicine itself via manufacturing it in nanoscale size range ( stabilized nanoscale crystals). Notably, the last FDA approval of such nanocrystal drug was in 2015, which is the drug for a rare progressive lung disease. In this article we will focus on some nanomedicines approved by the FDA in the last 5 years, as well as discuss promising ongoing clinical trials.
Nanotech in medicine: what is it for?
Nanomedicines are considered very effective in treating chronic diseases such as cancer, dementia, and diabetes as they fuel the metabolism of medications in the body. They deliver the drugs to the target site in the right proportion. The market's availability of nanomedical products such as DNA probes, nanosensors, and nanoparticle-based imaging agents is increasing the demand. However, the high cost associated with the nanomedicine manufacturing process and research and development activities may hinder fast nanomedicine market growth.
To concentrate more on the nanotechnology serving the precision drug delivery, it solves various issues of the conventional delivery systems, such as biodistribution and intracellular trafficking. Specifically, nanoparticles are aimed to increase the stability of transported active substances, pass the biological membranes and make the treatment overall safer and more efficient.
The clinical translation of the technology is getting slowed down for several reasons. Firstly, we don’t fully understand how the differences in physiology and pathology of various animal species compared to humans influence the behavior of nanoparticles in the body. Secondly, there are no two exactly the same patients, and this patient heterogeneity largely influences the effect of the nanoparticles, making the clinical outcome hard to predict and analyze.
According to some analytical sources, drug delivery applications dominated the market in 2021 and captured 30.23% of the overall market share. This segment is expected to maintain its dominance over the next five years. The rise in awareness about the benefits of nanomedicine in drug delivery applications and the increased prevalence of diseases drives the demand for nanomedicines for drug delivery applications.
A schematic image highlighting some biological barriers which nanoparticles can overcome, such as crossing epithelial barriers, organelle-specific intracellular delivery, navigating aggressive tumor microenvironment and targeting immune cells. Image credit: Nature Reviews (2021) (doi.org/10.1038/s41573-020-0090-8)
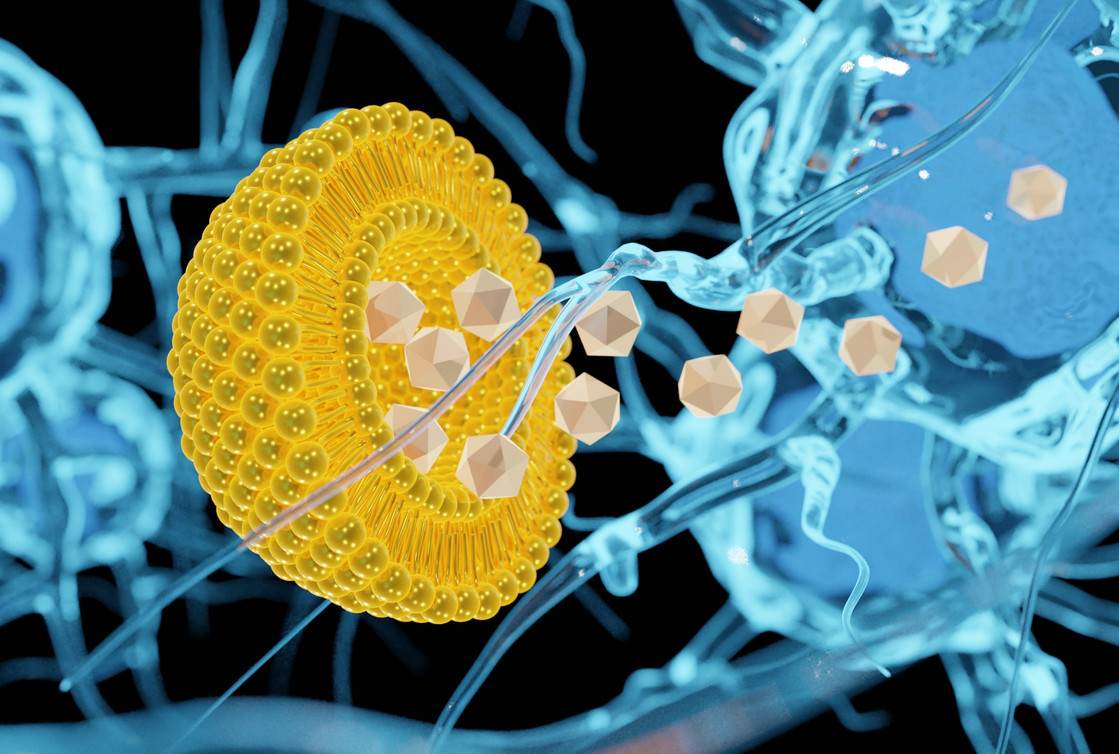
Lipid-based nanoparticles and liposomes
If we imagine the ball for some outdoor game, let’s say beach volleyball, we already have an imaginary prototype of the liposome -- a sphere composed of phospholipids with an “empty” space inside. Lipid-based nanoparticles (LNPs) are liposome-like structures, which have amphoteric properties and can deliver various drugs packed inside their “vacant empty space”.
Liposomes and LNPs can be engineered using diverse methods like reverse-phase evaporation, thin-film hydration, microfluidics technique, spray-drying and supercritical fluids technique. The advantages of LNPs as drug delivery carriers are the same as for liposomes: they are biodegradable, biocompatible, and are similar to lipids present in cell membranes, making them a non-toxic and non-damaging material for the human body. On the other hand, such nanoparticles can’t take much of the material to carry, meaning they suffer from a low drug loading, as well as they have a tendency to accumulate in the liver and spleen.
A schematic showing the liposome and LNP structure, with visible core architecture differences. Image credit: Exelead
Alnylam Pharmaceuticals
Alnylam, a biopharmaceutical company which is focused on developing RNA interference (RNAi) therapeutics, got the FDA and EMA approvals for their LNPs-packed drug in 2018. Onpattro™ (Patisiran) is the first ever approved small interfering RNA drug, as well as the first drug approved for the treatment of the polyneuropathy of hereditary transthyretin-mediated (hATTR) amyloidosis in adults.
The specific challenge of the double-stranded RNA (dsRNA) therapeutics is that such molecules are not supposed to get into the living cell -- they are immediately recognised as foreign, as a result of an evolutionary developed antiviral protection mechanism. That is why, according to the Alnylam scientists, “the most critical technical bottleneck in the development of RNAi drugs is how to achieve safe and efficient in vivo delivery”, so the dsRNA can be delivered precisely and efficiently to the targeted cells.
Liposomes and liposome nanoparticles are often specifically geared for the delivery of nucleic acid drugs, such as mRNA, miRNA, DNA oligonucleotides, siRNA and shRNA. This catered well to the technology of siRNA-based therapeutics of Alnylam, which couldn’t succeed without the well established delivery system, which happened to be liposome nanoparticles for their first approved drug.
Interestingly enough, after the approval of Onpattro, Alnylam did not continue their R&D activities in the direction of LNPs, because as they stated there are simpler and safer delivery technologies. Their next FDA approved drugs utilize N-acetylgalactosamine-conjugats delivery system, which works well for the targeted delivery to the liver cells -- hepatocytes.
Jazz Pharmaceutics
The previous example described how LNPs as drug delivery system work to secure the targeted delivery of the double-stranded RNA to the cells, whereas Jazz Pharmaceuticals uses their LNPs technology to reduce the dose-limiting toxicity and the overall safety for the anti-cancer drugs, improving the therapy outcome.
US-based Jazz Pharmaceuticals specializes mostly in developing treatments for the neurology and psychiatry markets, but also has oncology pipelines, getting an FDA approval in 2017 for their liposome encapsulated treatment for acute myeloid leukemia (AML). The fixed ratio combination of antineoplastic drugs daunorubicin and cytarabine for the AML treatment was already used in the clinics before, but the liposome encapsulation helped to address the specific group of high-risk AML patients, improving the survival rates and safety profiles.
In 2021 Jazz’s liposomal Vyxeos got an additional FDA approval for the treatment of newly-diagnosed therapy-related AML in pediatric patients 1 year and older. Even though the liposomal formulation still shares the long list of side effects with the original non-encapsulated combination, liposomal Vyxeos is comparatively safer and strictly cannot be substituted with the free drugs form using the same indicated dosages.
Polymer-based nanoparticles
Polymeric nanoparticles can be synthesized from both natural or synthetic materials, monomers and preformed polymers. In this case multiple nanoparticle features can be controlled in the manufacturing process, which can be emulsification, nanoprecipitation, microfluidics and more.
Depending on the architecture, polymeric nanoparticles can carry drugs inside the matrix or bound to the nanoparticle surface, which consequently defines the drug load and delivery capabilities. Since this type of nanoparticles is compatible with various types of drugs at the same time, it makes them a suitable tool for co-delivery applications. Most commonly, two forms of the polymer-based nanoparticles are used: nanocapsules and nanospheres, which differ in their structure and assembling process.
Additionally, polymeric nanoparticles are biodegradable and biocompatible, as well as relatively stable during the storage. However, even though this type of nanomedicines has a significant number of advantages, they suffer from the increased risk of particle aggregation and toxicity. This frequently results in the failure of clinical trials, but there are still numerous clinical candidates in the ongoing trials.
Novo Nordisk
Novo Nordisk, a Denmark-based pharmaceutical company focusing on hemophilia, growth disorders and obesity, got an FDA approval in 2017 for their hemophilia drug Rebinyn. It is the recombinant coagulation factor IX (FIX), which is PEGylated to increase its stability, forming a polymeric nanoparticle. PEGylation means the attachment of polyethylene glycol (PEG) polymer chains to the molecules of interest, which can be various drugs, vesicles, or a protein as in the case of Rebinyn.
In this case, the nanoparticles delivery system is critical to increase the half-life of the injected treatment, since the drug regulates the process of blood coagulation over time. It was demonstrated that the PEGylation of factor IX extends its half-life roughly 5 times compared to the non-modified form. Additionally, the Novo Nordisk team confirmed that the glycoPEGylation of FIX does not interfere with the primary and higher order structure of activated protein.
Flexion Therapeutics (acquired by Pacira Pharmaceuticals)
Having a narrow focus on long-lasting intra-articular injection therapies to treat osteoarthritis, a biotech company Flexion Therapeutics got the FDA approval for their drug in 2017, followed with the acquisition by Pacira Pharmaceuticals in October 2021.
Their FDA approved treatment Zilretta contains an active substance triamcinolone acetonide, which we might already know as a component of some dermatological creams. It is technically a corticosteroid -- hormone which reduces the inflammation, hence decreases some degenerative processes in tissues and the accompanying processes of swelling, itching etc. Considering the pathology of osteoarthritis (and rheumatoid arthritis as well) it is beneficial to use such antiinflammatory agents “right on site”, but there is a significant issue of rapid clearance of intra-articularly injected drugs.
To address the issue, Flexion used the polymeric nanoparticles technology for the controlled drug release over time after intra-articular injection. They apply a proprietary microsphere technology combining the corticosteroid drug with a poly lactic-co-glycolic acid (PLGA) matrix. This ensures prolonged treatment action and pain relief after the injection.
Notably, Pacira’s main focus is the liposome-based drug delivery systems, already owning an FDA approved drug -- bupivacaine liposome injectable suspension to fight the postsurgical pain. They developed a proprietary technology of multivesicular liposomes (pMVL) to encapsulate drugs, which is multidirectional in its applications, generally demonstrating the potential of nanoparticles in the drug development process.
Inorganic nanoparticles
Probably, one of the first examples which comes to mind speaking of inorganic nanoparticles is gold nanoparticles. Of course, the list is way longer, analyzing the market and ongoing clinical trials, which are blooming with superparamagnetic, gold, manganese, silica nanoparticles and more. Often, the inorganic nanoparticles studies are directed towards cancer therapy, having less variety than two previously described groups.
The distinguishing feature of inorganic nanoparticles is uniqueness of electric, magnetic and optical properties, combined with a variety of particle architecture (including size, structure and geometry). The combination of these parameters can be used to find unique theranostic agents for specific needs. However, not all needs can be satisfied, since inorganic nanoparticles have toxicity and solubility limitations.
Gold nanoparticles are one of the most well studied in this category, they are used as nanospheres, nanoshells, nanostars and nanocages. Additionally, they can be easily functionalized, granting them additional properties for the advanced delivery capabilities. At the same time, magnetic iron oxide nanoparticles showed some success as contrast agents, thermal-based therapeutics and drug-delivery systems.
Nanobiotix
One of the most recent approvals to observe in the field of inorganic nanoparticles is hafnium oxide nanoparticle by Nanobiotix, a France-based company which develops nanomedicine programs for the local cancer treatment. The drug called Hensify is a radioenhancer, which got European market approval in 2019 for the treatment of locally-advanced soft tissue sarcoma.
Prior to standard radiotherapy Hensify should be injected directly into a malignant tumor, where nanoparticles accumulate in cancer cells in clusters, driven by their accordingly chosen properties. Nanoparticles remain inert unless interacting with ionizing radiation; once activated, hafnium oxide nanoparticles should increase the energy absorbed from radiotherapy and enhance the dose delivered.
The specificity of the drug in this case is ensured by the direct injection into the tumor site, and according to Nanobiotix there is no leakage into the surrounding tissues, meaning no effect on the healthy cells. This highlights the restriction of such an approach -- the site of the injection should be reachable, so the precision can be sufficiently high.
Notable clinical trials to watch
Celsion Corporation
Celsion is a clinical stage biotechnology company focused on advancing a portfolio of innovative cancer treatments, including immunotherapies and DNA-based therapies. Both of their leading products utilize the nanoparticles delivery system.
ThermoDox is a Celsion’s advanced clinical candidate, developed to treat primary liver cancer with a very well known active compound, but in a very elegant way. The technology is based on lysolipid thermally sensitive liposomes (LTSL) -- a heat controlled system for the drug release, which in case of ThermoDox is combined with a standard chemotherapy drug doxorubicin.
The “magic trick” is that these liposomes are composed of lipid molecules that quickly change structure when heated to a temperature of 40-45°C, creating channels in the liposome bilayer that allow encapsulated drug to be rapidly released into the surrounding tissue. As a result, LTSL technology enables delivery of higher concentrations of chemotherapy drugs directly to the tumor, as in case of ThermoDox it was shown to deliver 25 times more doxorubicin into tumors compared to the intravenous infusion.
Celsion’s scientists state that the strength of LTSL technology is also based on one of the cancer hallmarks: the fact that the tumor vasculature is usually severely damaged, having disrupted architecture with multiple blunt ends and leakages. This leaking is used as a “tumor gate” for the liposomes, which get inside and stay there until activated for the drug release. Additionally, the local application of heat increases the liposomes intake by the tumor tissue even more.
The phase III of clinical trials for ThermoDox was completed showing the positive results (a significant increase of the survival rate compared to the radiofrequency ablation used without encapsulated doxorubicin), so it is highly probable to see ThermoDox among the FDA approved treatments soon.
Nektar Therapeutics
Nektar Therapeutics is known as a biopharmaceutical company with an R&D pipeline of investigational medicines in oncology, immunology, and virology. They own a polymer conjugate chemistry technology platform, which is geared for targeting the tumor tissue, tuning receptor selectivity of immune cells and extending the half-life of drugs.
In 2021 they finished the phase III of clinical trials for one of their drug candidates -- NKTR-102, targeted towards metastatic breast cancer, specifically with brain metastases. Previously, the drug wasn’t granted the marketing authorisation by EMA in 2017.
Nektar’s drug has an active compound irinotecan (topoisomerase inhibitor), linked by carboxymethyl glycine and polyethylene glycol (PEG) chains to a central pentaerythritol ether. This polymeric nanoparticle modification allows to significantly extend the half-life of the drug, according to the company. Even though the clinical trials were promising at first, they overall demonstrated only slight improvement of the patient’s survival rates, which was not significant enough to meet the approval criteria.
Nektar has multiple other clinical candidates utilizing their nanoparticle technology, which will hopefully show a higher efficiency rate at the clinical trials.
Enceladus in collaboration with Sun Pharma Global
An India-based generic pharmaceutical company Sun Pharma collaborated with Enceladus, a spin-off from Utrecht University, to develop treatment for rheumatoid arthritis flares. The phase III of clinical trials was terminated in November 2021, and the results were discussed in their article published in 2022.
The treatment was based on intravenous injections of Nanocort -- PEGylated liposomal prednisolone (glucocorticoid), as a long-lasting anti-inflammatory drug. Both PEGylation and liposomal encapsulation are supposed to increase the half-life of prednisolone, hence improving the clinical outcome for rheumatoid arthritis flares.
According to the clinical trials results, Nanocort showed to be more effective in reducing the flares compared to the intramuscular injections of glucocorticoids (current standard of care). The difference was also significant, showing the potential for the Nanocort approval. However, even though Nanocort has similar safety compared to other common glucocorticoid treatment (Depo-Medrol), it had a higher incidence of hypersensitivity reactions during liposome infusion. This is not an unexpected issue for nanoparticle-based drugs, and probably a “price to pay” for other advantages.
Conclusion
The market of nanomedicines continues actively expanding with new clinical candidates, approaches and approvals. Nanoparticles for drug delivery are becoming a “golden standard”, since they can assist in passing biological barriers, targeted delivery to the tissue or even organelles, increase the stability of transported active substances and control the release of the drug.
The majority of globally marketed nanomedicines belong to the oncology category, followed by hematology. But nanoparticles serve various other fields, such as neurology, metabolic and autoimmune diseases, vaccines etc. Even the recently approved vaccines for COVID-19 by Pfizer Pharmaceuticals and by Moderna use lipid nanoparticle encapsulated mRNA, demonstrating the broad potential of the technology.
In the future we would expect a larger shift from the oncology field towards other directions, because now the majority of nanoparticles are still developed for cancer treatment. Currently, one of the main reasons for the nanomedicines failure remains to be an intolerable toxicity (which is usually or detected at the phase I of clinical trials). At the same time, patient selection is critical for the trial's outcome, for example when dealing with a highly heterogeneous cancer it can have a major impact on the results. Hopefully, the advances in nanotechnology and optimization of clinical trials using artificial intelligence can speed up the approval of new nanomedicines.
References
-
Halwani AA. Development of Pharmaceutical Nanomedicines: From the Bench to the Market. Pharmaceutics. 2022 Jan 3;14(1):106. doi: 10.3390/pharmaceutics14010106. PMID: 35057002; PMCID: PMC8777701.
-
Shan X, Gong X, Li J, Wen J, Li Y, Zhang Z. Current approaches of nanomedicines in the market and various stage of clinical translation. Acta Pharm Sin B. 2022 Jul;12(7):3028-3048. doi: 10.1016/j.apsb.2022.02.025. Epub 2022 Mar 1. PMID: 35865096; PMCID: PMC9293719
-
Mitchell, M.J., Billingsley, M.M., Haley, R.M. et al. Engineering precision nanoparticles for drug delivery. Nat Rev Drug Discov 20, 101–124 (2021). https://doi.org/10.1038/s41573-020-0090-8
Topic: Next-Gen Tools