Infinitus Partners with IBM Consulting to Automate Patient Access with AI Agents
Infinitus, a San Francisco–based company focused on conversational AI for healthcare administration, has partnered with IBM Consulting, the professional services arm of IBM that advises on large-scale technology transformation, to deploy agentic AI systems in specialty pharmacy and other healthcare workflows. The collaboration targets high-volume administrative and clinical tasks such as benefit verification and prior authorization, which are frequent bottlenecks in patient access to therapies.
Infinitus’ platform is built around its digital assistant, Eva, which automates payor-facing calls and delivers structured data outputs in real time. The system is reportedly trained on more than 1,000 therapies and supports interactions with over 200 major payors, adapting to changing coverage requirements through continuous learning.
Eva handles some of the most repetitive administrative work in specialty pharmacy—confirming insurance coverage, following up on prior authorizations, and managing prescription transfers. Instead of returning raw call logs, it captures structured details like plan information, approval status, claims data, and savings eligibility.
According to Infinitus, Eva draws on experience from over a million payor calls and uses standardized workflows to outperform manual callers by 10% in accuracy. The goal is to speed up time to therapy, help pharmacies handle more cases without extra staff, and flag patients who might qualify for financial support. The platform is designed for enterprise use and meets HIPAA and SOC 2 security standards.
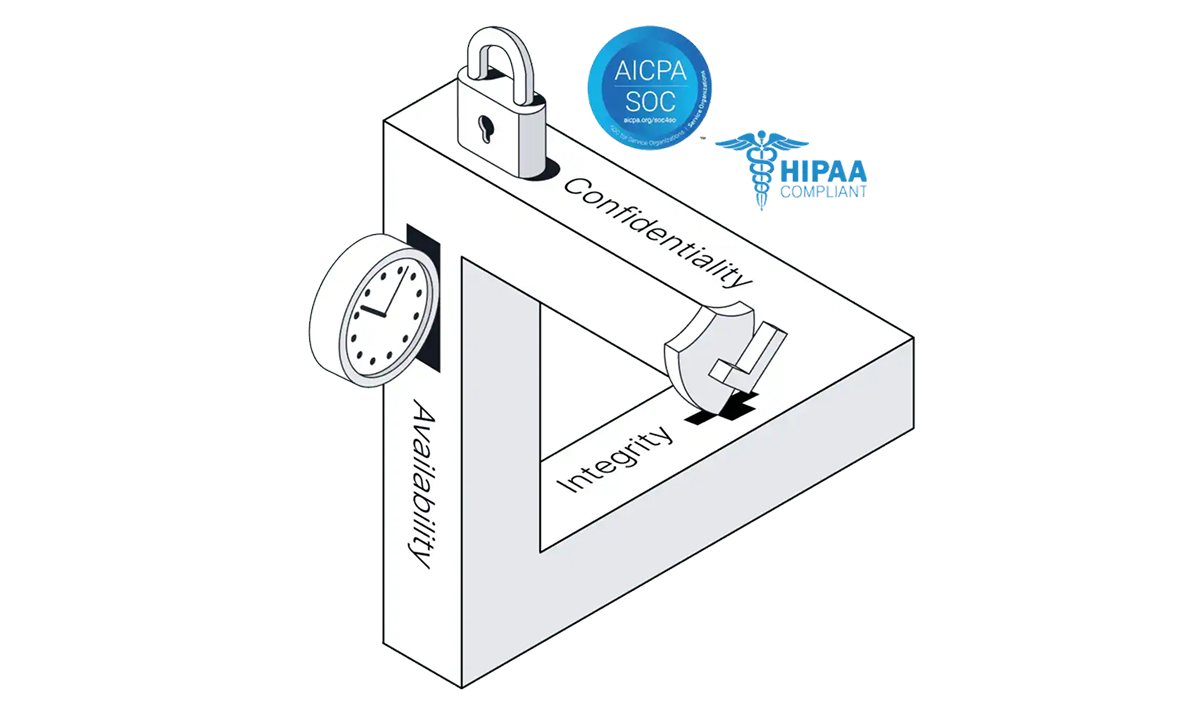
Image credit: Infinitus
A case study from a national payor-owned specialty pharmacy shows how the organization adopted Infinitus’ AI agents to automate benefit verifications, first for home health products and later across hundreds of medications. According to Infinitus, its platform completed more than 60,000 benefit verification and prior authorization follow-up tasks for this major specialty pharmacy in the first half of 2025.
Reported results included an average of 29 minutes unlocked per benefit verification call and 20 minutes per prior authorization status call, a 314 percent year-over-year increase in benefit investigations without added staff or technology, and a 98 percent success rate in benefit verifications. The company positions its system as a way to streamline communications between providers, pharmacies, and payors, while maintaining the security and compliance standards required in healthcare.
The firms state that their collaboration is designed to reduce cycle times in pharmacy workflows, accelerate patient access to therapy and financial assistance programs, and improve the reliability of AI-driven interactions in regulated healthcare settings.
We track collaborations like this weekly in Where Tech Meets Bio—our newsletter on startups, platforms, and deals at the intersection of biotech and digital.
Topic: Tech Giants